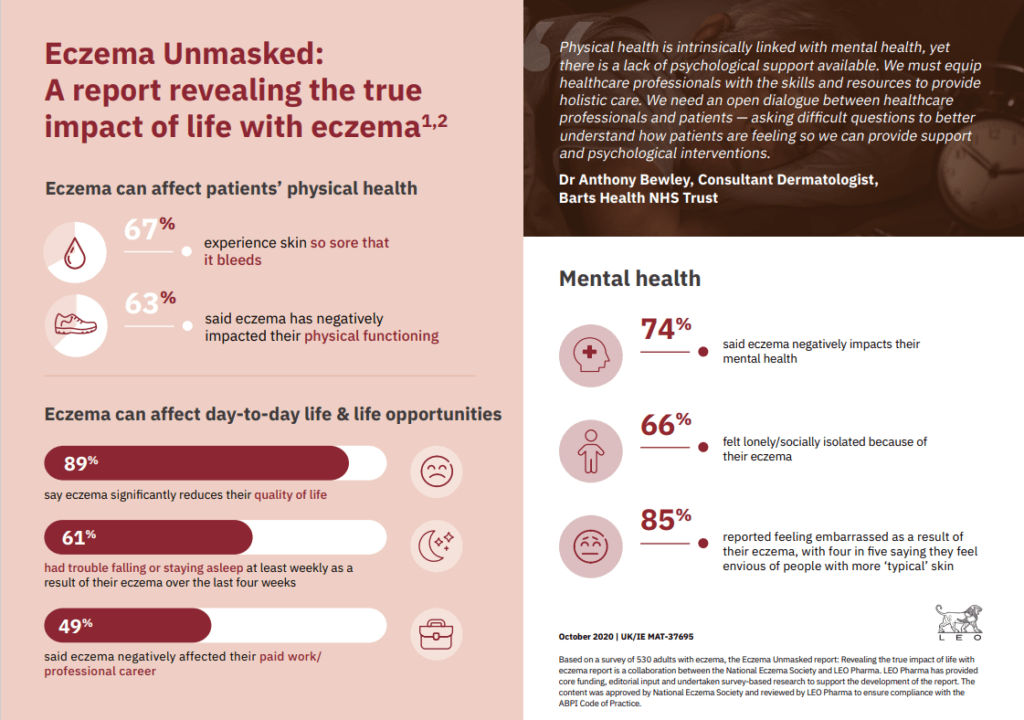
89% of adults reveal significant impact on quality of life1 ~ new report amplifies the voices of people living with eczema; urging healthcare professionals to provide holistic care and commissioners to fund appropriate service delivery to drive better outcomes
A new report developed by the National Eczema Society, in collaboration with and with funding from LEO Pharma, launches today, with insights from over 1,000 people affected by the condition in the UK. Eczema Unmasked raises awareness of the extensive and under-recognised impact eczema can have on all aspects of peoples’ lives including physical health, mental health, quality of life and long-term life opportunities – highlighting the variation in healthcare provision and measures that must be taken to bridge these gaps in care.
Based on these findings, LEO Pharma and the National Eczema Society want to strengthen the voices of those living with eczema; calling for the development of clinical guidelines and quality standards for adults and adolescents with eczema, and to improve access to appropriate care and services.
Impact on quality of life:
- 89% say eczema significantly reduces their quality of life;1 experiencing painful and variable physical symptoms which are difficult to manage with current treatments
- 67% experience skin so sore that it bleeds1
- 61% say they had trouble falling or staying asleep at least once a week over the last four weeks1
- 59% say eczema negatively affected their sexual intimacy1
- 61% say eczema affected their social life1
- 49% said eczema negatively affected their paid work/professional career1
“I have lived with severe eczema for decades and, over what is perhaps now hundreds of consultations, have rarely been asked ‘How are you feeling?’ In my experience the health impact of eczema is not well understood or addressed.”
- Anon, male living with eczema for over 30 years
Impact on mental health
74% of patients said eczema negatively impacts their mental health.1 The unrelenting cycle of itchy and painful skin and wider impact on everyday life can take an emotional toll, leaving many patients depressed or sad (76%), anxious or nervous1 (79%) and lonely / socially isolated (66%).1 Despite this, over 50% of patients had never been offered psychological interventions by their NHS doctor to help them cope.1
“Physical health is intrinsically linked with mental health and yet there is a worrying lack of psychological support available to people living with skin conditions like eczema,” says Dr Anthony Bewley, Consultant Dermatologist, Barts Health NHS Trust. “There is an urgent clinical need to equip healthcare professionals with the necessary skills and resources to provide the holistic care that patients need. We need an open dialogue between healthcare professionals and patients – asking difficult questions to better understand how patients are feeling so we can provide necessary support and psychological interventions.”
Lack of clinical guidelines and quality standards
Despite the significant negative impact of eczema on patients’ quality of life, 39% felt let down by healthcare professionals about their treatment1 and 27% feel healthcare professionals don’t take their eczema seriously enough.1 The findings reveal considerable variation and gaps in healthcare provisionwith60% having no care plans in place,1 highlighting the challenges faced by patients and healthcare professionals in managing a complex, variable condition – leaving people disillusioned.
“There are no National Institute for Health and Care Excellence (NICE) clinical guidelines and quality standards to guide diagnosis and management of eczema in adolescents or adults, leading to huge variations of care. Greater standardisation in clinical care driven by evidence-based treatment guidelines is desperately needed to improve patient outcomes, guide commissioning decisions and prioritise healthcare resources effectively.” says FunmiOluwa, Market Access & External Affairs Director UK/IE at LEO Pharma.
There are concerns about waiting times for GP referrals to secondary care as 35% of patients (42% for adults with moderate, severe or very severe eczema) say on the last occasion they were referred to a dermatologist, they waited over three months for an appointment, with 14% waiting more than six months.1 Nearly one third (29%) often have difficulty obtaining emollients on NHS prescription1 and over one quarter (28%) with moderate, severe or very severe eczema often experienced challenges obtaining a biologic treatment to manage their eczema.1
“Due to a lack of undergraduate and postgraduate training, often coupled with inadequate local resources, sadly many GPs are not always equipped to cope with the full needs of people living with a complex condition like eczema,” says Dr George Moncrieff, Dermatology Clinical Lead SDS MyHealthCare Federation Birmingham / past chair Dermatology Council England. “There’s critical need to address these education and service gaps as we know that up to a quarter of all GP consultations include an element of dermatology yet, astonishingly, this is still not considered a priority.”
Expectations and opportunities for managing eczema
“It’s important to better understand the full impact of living with eczema and for patients to get the treatment and support they need to manage this painful medical condition. These survey responses show just how tough it can be living with eczema,” says Andrew Proctor, Chief Executive of the National Eczema Society.
The Eczema Unmasked report highlights three key calls to action:
- Strengthen the voices of those living with eczema
- Raise public awareness of life with eczema and dispel the myth that it’s just a minor skin complaint
- Empower people to talk about their eczema to break out of the isolation
- Give people confidence to press for the medical care and support they need
- Provide evidence and deeper understanding of eczema for healthcare professionals to improve patient outcomes through holistic approaches to care
- Develop clinical guidelines and quality standards for adults and adolescents with eczema
- There are no National Institute of Health and Care Excellence (NICE) clinical guidelines and quality standards to guide diagnosis / management of adults or adolescents living with eczema – impacting on costs to the health economy
- Absence of frameworks leads to huge variations of care at primary and secondary care levels, with healthcare professionals relying on individual knowledge and clinical judgement
- Greater standardisation in clinical care driven by evidence-based treatment guidelines is desperately needed to improve patient outcomes
- Frameworks will be critical to guide commissioning decisions and prioritise healthcare resources effectively – ensuring consistent access to optimal care and treatment
- Improve access to appropriate care and services
- Dermatology represents an important part of NHS provision, yet fundamental barriers to accessing appropriate care and services still exist
- Urgent need to improve knowledge of skin diseases and wider impact on patients within primary care
- Bridge the gap between specialist and primary care services – patients referred to the right service, in the right place, at the right time, so no patient is left untreated or unsupported
- Encourage clinicians, commissioners and policymakers to prioritise and fund effective care and services locally to reduce unnecessary variation in care and knowledge
LEO Pharma and the National Eczema Society’s ‘Eczema Unmasked’ report aims to better represent the experiences of adults with eczema and serve as a new, robust evidence base to demonstrate how eczema can significantly impact people’s physical health, mental health, their quality of life, long-term life opportunities and access to appropriate care.
To access the full ‘Eczema Unmasked’ report visit: http://bit.ly/EczemaUnmasked
References
- Savanta: ComRes. LEO PHARMA AND NATIONAL ECZEMA SOCIETY – ECZEMA UMASKED – ADULTS. Available at: https://www.leo-pharma.co.uk/EczemaUnmasked-adultsdata (Accessed October 2020).
UK/MAT-39479 | October 2020